Introduction of modern technologies for sterilization and disinfection of instruments
Authors
Bichul Yuliia Vladimirovna

Share
Annotation
The article discusses modern technologies for sterilizing and disinfecting medical instruments in order to improve the effectiveness and safety of medical procedures. It analyzes the main methods of sterilization, such as steam, gas, chemical, and ultraviolet treatment, as well as innovative tools and equipment that help to optimize disinfection processes. Special attention is given to automation of procedures and quality control, which helps to reduce the risk of infection and increase the lifespan of instruments. Regulatory requirements and recommendations from the World Health Organization (WHO) are taken into consideration, as well as the potential for introducing new technologies into clinical practice
Keywords
Authors
Bichul Yuliia Vladimirovna

Share
Introduction. Today, the use of modern technologies for the sterilization and disinfection of instruments is a crucial task in the healthcare sector. It is aimed at ensuring the highest level of safety for patients and medical staff.
With an ever-increasing number of infectious diseases and microorganisms becoming resistant to traditional disinfection methods, the importance of developing and implementing innovative approaches has grown significantly. Effective sterilization and disinfection not only prevents cross-infection but also contributes to the longevity and functionality of medical equipment.
Modern technologies include the use of various techniques and substances, such as steam under pressure, gas treatments with ethylene and hydrogen peroxide, and ultraviolet radiation. Automated process control systems are also used to ensure accuracy and efficiency.
The implementation of these technologies requires strict adherence to regulatory standards and a comprehensive approach, encompassing the selection of the most appropriate method, proper upkeep of equipment, and qualified monitoring of outcomes. The introduction of advanced sterilization and disinfection techniques is becoming a crucial factor in enhancing the quality of healthcare services, reducing the risk of hospital-acquired infections, and ensuring the long-term sustainability of the healthcare system.
Discussion. It is worth noting that the history of the development of sterilization and disinfection techniques for instruments has gone through several important stages. Each stage reflects the advances in science and medicine in the fight against infections and the protection of patients.
In earlier times, people used primitive methods to clean tools, such as burning them on fire, boiling them in water, or treating them with smoke or herbal smoke. These methods somewhat reduced the number of harmful microorganisms, but they did not guarantee complete destruction of the infectious agents.
A key turning point in the history of sterilization was the discovery of microbiology in the XIX century. Scientists such as Louis Pasteur and Robert Koch proved that microorganisms were the cause of infectious diseases. This discovery led to the development of systematic methods for sterilization and disinfection, which have since become an essential part of medical practice.
During this time, boiling, steam sterilization, and the use of disinfectants such as chlorine and phenols were introduced. These methods were instrumental in preventing the spread of diseases and saving countless lives.
With the development of technology in the XX century, new methods of sterilization emerged. Steam pressure sterilization (autoclaving), introduced at the beginning of the century, became the gold standard due to its efficiency and safety. This method allows the destruction of all types of microorganisms, including bacterial spores, through exposure to high temperatures and steam under pressure.
Alongside this, chemical disinfection methods developed, utilizing more advanced antiseptic and disinfectant agents such as alcohols, halogen-containing substances, aldehydes, and hydrogen peroxide. Later on, gas sterilization techniques using ethylene oxide were introduced, becoming essential for the treatment of heat-sensitive medical instruments.
In recent decades, there has been a focus on modern technologies such as plasma sterilization, ultraviolet irradiation, and low-temperature peroxide treatment. These methods offer effective disinfection while minimizing damage to instrument materials, significantly expanding the capabilities of medical equipment.
The development of these sterilization technologies reflects the advancement of medical science and technology. We have moved from simpler and less reliable methods to more complex, highly efficient, and safe approaches that meet the modern requirements for infection control in hospitals and clinics [2].
Microbiological risks in nail salons can pose a potential threat to the health of clients and staff, as there is a possibility of transmission of pathogenic microorganisms through tools, surfaces, and skin contact. These risks are linked to the presence and spread of bacteria, viruses, and fungi, which can cause various infectious diseases [1]. According to the classification of the World Health Organization (WHO), microorganisms can be divided into four categories of pathogenicity, as shown in Table 1.
Table 1 - Classification of pathogenic microorganisms
|
Group |
Examples of microorganisms |
Characteristic |
|
I |
Bacillus subtilis |
Low pathogenicity, minimal risk to healthy individuals. |
|
II |
Staphylococcus aureus, Escherichia coli |
Moderate pathogenicity, with possible diseases associated with impaired immunity. |
|
III |
Mycobacterium tuberculosis, Hepatitis virus |
High pathogenicity and serious diseases require special working conditions. |
|
IV |
Ebola virus, Marburg virus |
Very high pathogenicity and deadly diseases work only under conditions of maximum biosafety. |
It should be noted that modern technologies for sterilization and disinfection of instruments provide a range of methods that effectively destroy microorganisms and enhance the safety of medical procedures. Some of the most commonly used methods include autoclaving, gas sterilization, plasma sterilization, and chemical disinfection, as well as innovative techniques based on ultraviolet radiation (Fig. 1).
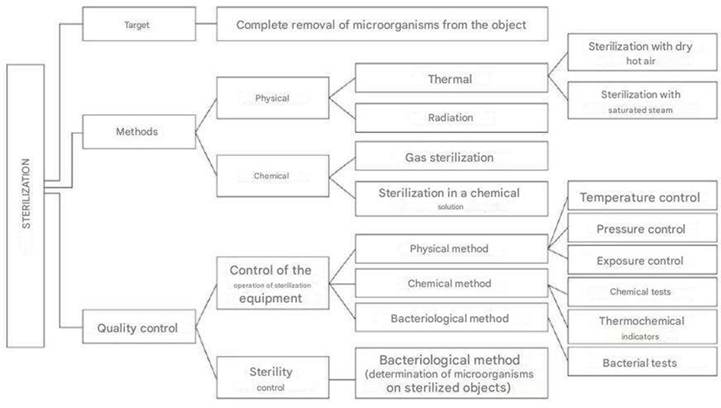
Fig. 1 - Sterilization methods and their advantages
Autoclaving is the most common method of sterilization. It operates by exposing materials to saturated steam under high pressure and at a temperature between 121°C and 134°C. This process destroys bacteria, viruses, fungi, and their spores. Autoclaving has a high level of reliability and is suitable for sterilizing metal, glass, and heat-resistant materials. It is widely used in surgical and dental procedures, as well as in laboratories.
Ethylene oxide gas sterilization is another method used to treat heat-sensitive instruments, plastic, and rubber products. It works at lower temperatures (between 37°C and 63°C) and can penetrate packaging and hard-to-reach areas of instruments. However, this method requires special safety precautions due to its toxicity and the need for aeration after the procedure.
Plasma sterilization is a method that uses reactive oxygen species and ozone produced in low-temperature plasma to kill microorganisms. This process is environmentally friendly and effective against a wide range of pathogens, including spores, making it ideal for sterilizing delicate materials and electrical equipment.
Chemical disinfection involves the use of solutions containing glutaraldehyde, hydrogen peroxide, and chlorhexidine, among other antiseptic substances. This method can be used for pre-treatment and in situations where thermal sterilization cannot be applied. To ensure its effectiveness and safety, it is important to follow the correct concentration and exposure times.
Ultraviolet (UV) irradiation uses short-wavelength UV light (around 254 nanometers) to destroy the DNA of microbes, preventing their ability to reproduce. This technique can be used to disinfect surfaces, air, and occasionally tools, often in combination with other methods for enhanced effectiveness [3].
Modern sterilization and disinfection techniques offer a range of effective methods that ensure a high level of safety when handling medical instruments and help prevent the spread of infection. The choice of technique depends on the type of instrument, material, and operating conditions.
Results. In our opinion, modern sterilization and disinfection technologies, despite their high efficiency and variety of methods, face several challenges that affect the quality and safety of the procedures. These challenges include technical, economic, organizational, and environmental issues.
One of the main challenges is the complexity and high cost of equipment. Many modern techniques, such as plasma sterilization and ethylene oxide gas treatment, require specialized and expensive equipment. This makes them difficult to implement in medical facilities with limited budgets, especially in areas with poor infrastructure.
The second important aspect to consider is the sensitivity of certain materials to sterilization methods. Some tools that are thermally or chemically unstable can deform, lose their functionality, or interact in a toxic way with the reagents used. For instance, an autoclave may not be suitable for heat-sensitive plastics, and ethylene oxide residue requires prolonged aeration in order to avoid harming patients and staff.
A third challenge is ensuring that strict sterilization protocols and quality control measures are followed. Inadequate training of personnel, human error, non-adherence to processing times and concentrations of chemical disinfectants, can lead to incomplete elimination of infectious agents, increasing the risk of cross-infection. The absence of regular monitoring of equipment functionality and sterility testing also has a detrimental effect on safety.
The fourth issue relates to the time required for the procedure and its complexity. Some methods involve a lengthy treatment cycle and subsequent aeration, such as with ethylene oxide, which can slow down work processes and reduce the capacity of medical facilities. Additionally, rapid methods are often limited in terms of their range of effects and scope of application.
Furthermore, environmental and safety concerns arise from the use of toxic and hazardous substances. Ethylene oxide and certain chemical disinfectants must be carefully disposed of and monitored, as they have the potential to cause contamination and harm to personnel's health.
Despite the high efficiency of modern sterilization and disinfection techniques, their use still faces various technical, economic, organizational, and environmental challenges that require an integrated approach and competent management. It is essential to improve equipment and techniques in order to overcome these challenges.
Therefore, an integrated and systematic approach is necessary to address the technical, economic, organizational, and environmental issues associated with modern sterilization and disinfection methods.
First and foremost, it is essential to optimize the choice of technology based on the type and material of the instrument. For thermosensitive products, gentle methods such as low-temperature chemical sterilization, plasma installations, or peroxide systems are advisable, as they minimize the risk of damage. Scientific research is also needed to develop new materials that can withstand sterilization and are compatible with modern processing techniques.
In order to address the issue of the high cost of equipment and maintenance, public and private initiatives should be promoted to modernize medical facilities. Purchases of certified equipment should be encouraged, taking into consideration their energy efficiency and ease of use. The introduction of modular and automated systems can reduce processing time and lower staffing requirements.
Training and advanced training for medical personnel are essential for ensuring the proper and effective use of sterilization and disinfection techniques. Regular training sessions and control checks can help minimize errors caused by the human factor. Implementing a quality control system and process validation will ensure consistency in sterility.
To speed up processing time and increase productivity, it is worth considering combining different methods and implementing optimized protocols tailored to specific circumstances and equipment types. Research into accelerated sterilization cycles and improved equipment will reduce downtime.
Environmental problems are being addressed with less toxic and biodegradable disinfectants, as well as the implementation of waste treatment and neutralization technologies. Modern ventilation and heat recovery systems reduce the harmful effects on staff and the environment.
Strict control and regulation of the handling of hazardous substances ensure the protection of human health and environmental safety. The solution to these challenges is possible through a combination of innovative technical solutions, skilled management, staff training, and the development of regulatory frameworks that will improve the quality and safety of instrument sterilization and disinfection in medical practice.
Conclusions. Modern methods of sterilization and disinfection play a crucial role in ensuring the safety of medical procedures and preventing infectious diseases. The choice of optimal technology depends on the type and material of tools being processed, as well as on the specific characteristics of the institution.
High efficiency and reliability can only be achieved with the right combination of equipment, chemicals, and strict adherence to protocols. This requires constant monitoring and skilled personnel. While the economic aspect is significant, the introduction of advanced technologies often involves high costs for equipment and training. However, these expenses are justified by reducing the risk of infection, shortening treatment time, and enhancing patient safety.
The environmental challenges associated with the use of toxic disinfectants and the generation of hazardous waste call for a transition to safer and more environmentally friendly technologies. This requires a systematic approach to waste management and environmental control, as well as the development of a regulatory framework and introduction of innovative solutions.
By implementing these measures, we can minimize the negative impact of disinfection processes on staff health and the environment. Success in this field is only possible through an integrated approach that includes technical solutions, scientific research, organizational measures, and legislative regulation. This approach will ensure high-quality healthcare, reduced infection risks, and environmental safety in accordance with modern healthcare standards.
References:
Disinfection and sterilization of instruments in the manicure room [Electronic resource]. – Access mode: https://cosmake.by/blog/sovetypokupatelyam/dezinfektsiya-i-sterilizatsiya-instrumenta-v-manikyurnom-kabinete
Ostrovskaya N. Disinfection and sterilization in hairdressers, manicure rooms, cosmetology, beauty and health centers // SES: Sanitary and epidemiological interlocutor, 2008, No. 7, pp. 6-9.
Turgeneva I.A., Brusina E.B., Gromova V.A., Averyanova M.M. Problems of anti-infective protection in beauty and health institutions // Medicine in Kuzbass. - 2005. – Vol. 4, No. 4. – pp. 209-211.